All too often do I feel like my voice is the only one acknowledging + championing the need to heed the emotions, the wider human experience, of people in healthcare. ALL people, be it workers, patients, friends, families, bystanders.
Yet last week I found myself in the rare, yet inspiring and reaffirming, space of hearing myself in the words, through the voices, of multiple people in the room! I attended Make Birth Better’s (MBB) 10th Annual Birth Trauma Summit in London on 13th May 2025 (click here for more information), and me taking the time to write this up is testimony to how powerful I found this event to be.

Make Birth Better
MBB is an organisation that was founded 10 years ago with the mission to raise awareness and prevent perinatal trauma through campaigning, training and support. I only learnt about their work recently, and attended The Birth Trauma Training Programme they provide (click here for more information) before this summit. The progress MBB have been involved with these last 10 years has been incredible, and the ambitions they have for the future sound both vital and exciting.
What is perinatal trauma, and why are you interested in this?
Perinatal trauma encompasses a range of distressing events experienced by individuals surrounding fertility, pregnancy, childbirth, or related experiences, which can include loss, complications, injuries, negligence, insufficient consent and support. Consequences can range from being short-lived to lifelong for people.

I have witnessed and encountered this in myriad forms in my personal and professional life, and will continue to do so. My experiences, and those many have shared with me, have demonstrated not only how frequent and extensive perinatal trauma is, but also how paramount it is that we acknowledge the wider human experience of “medical/care” events. The importance of giving time and agency to what people think, how they feel, their values and beliefs, in their experience of medical/care events, can’t be understated. In short, this understanding can help prevent errors, deaths, trauma, suffering, injury and more for providers and recipients of care, and enable us all to manage these events better when they do occur and thereafter.

Take aways
I want to sit down and take the time to absorb and explore much of the rich content from this summit, but here are some key points and take aways for me:
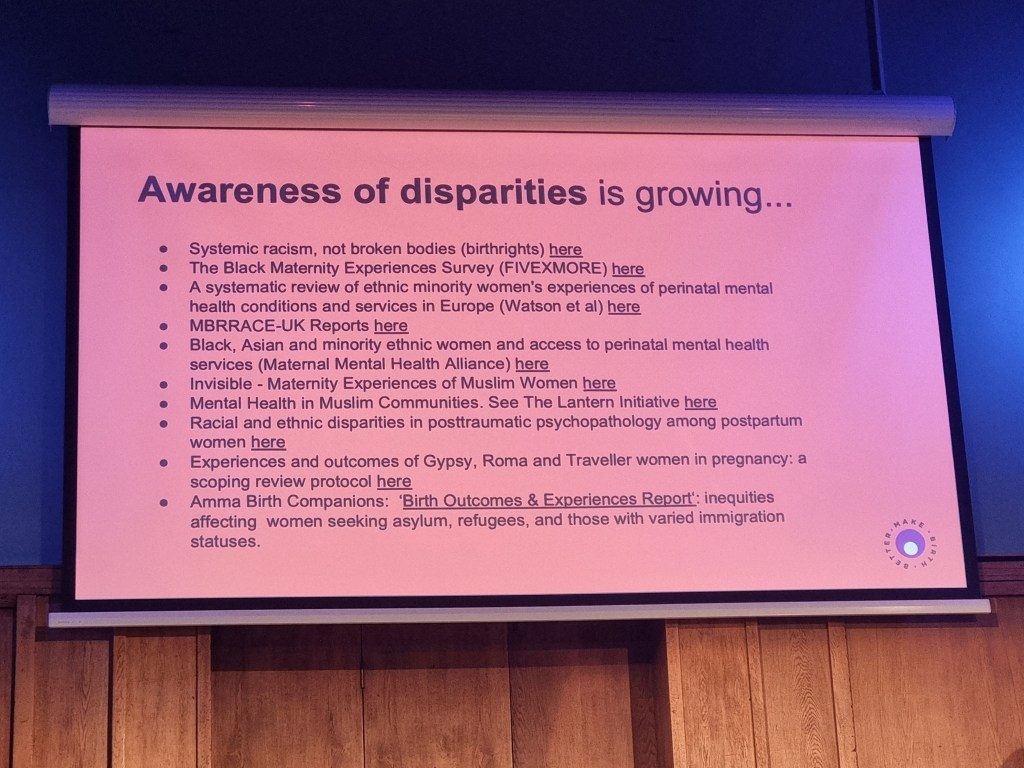
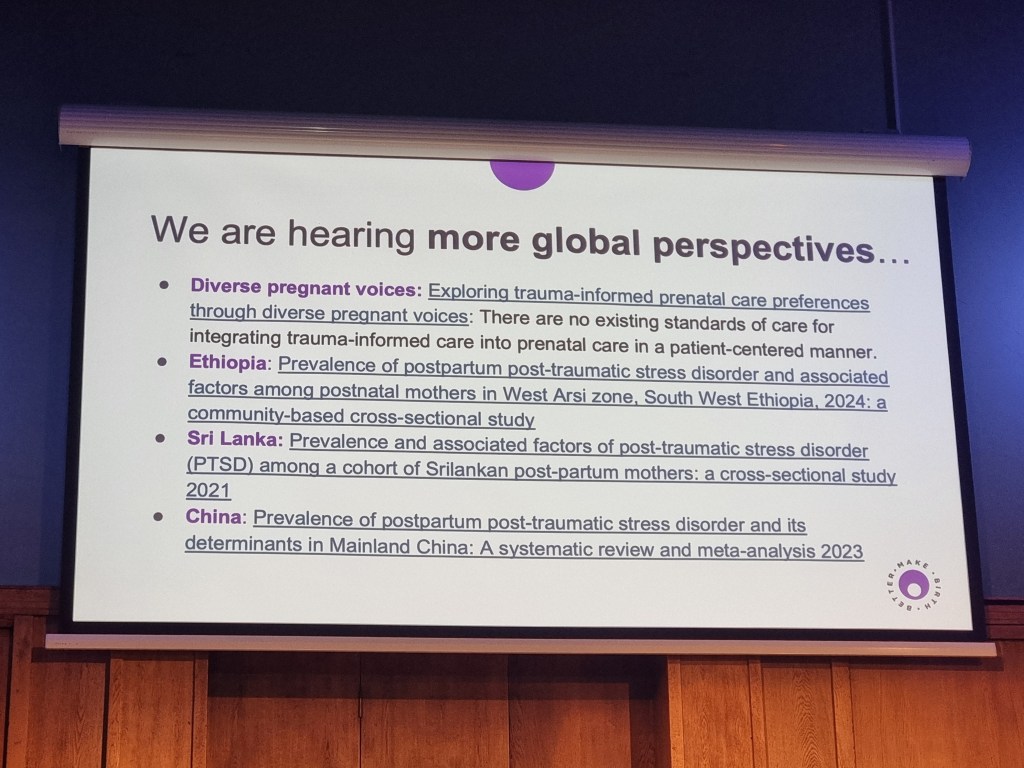
1) Developments to date – there have been some milestone achievements affecting multiple guidelines and institutions, but the key one has to be RECOGNITION of the existence and significance of perinatal trauma. The 2024 Birth Trauma Inquiry in the UK is certainly a landmark achievement (click here for more information) in enabling greater recognition, whilst I’m particularly keen on monitoring the future progress of the INTERSECT Study, which is looking at global patterns and trends of childbirth-related PTSD and trauma (click here for more information).
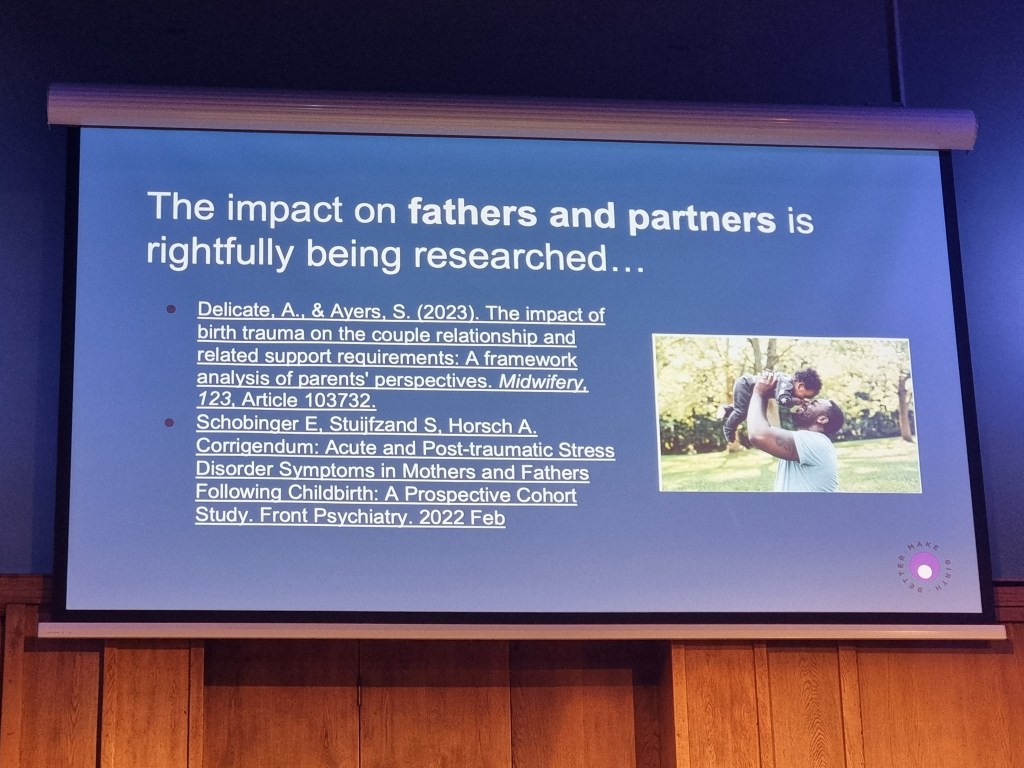
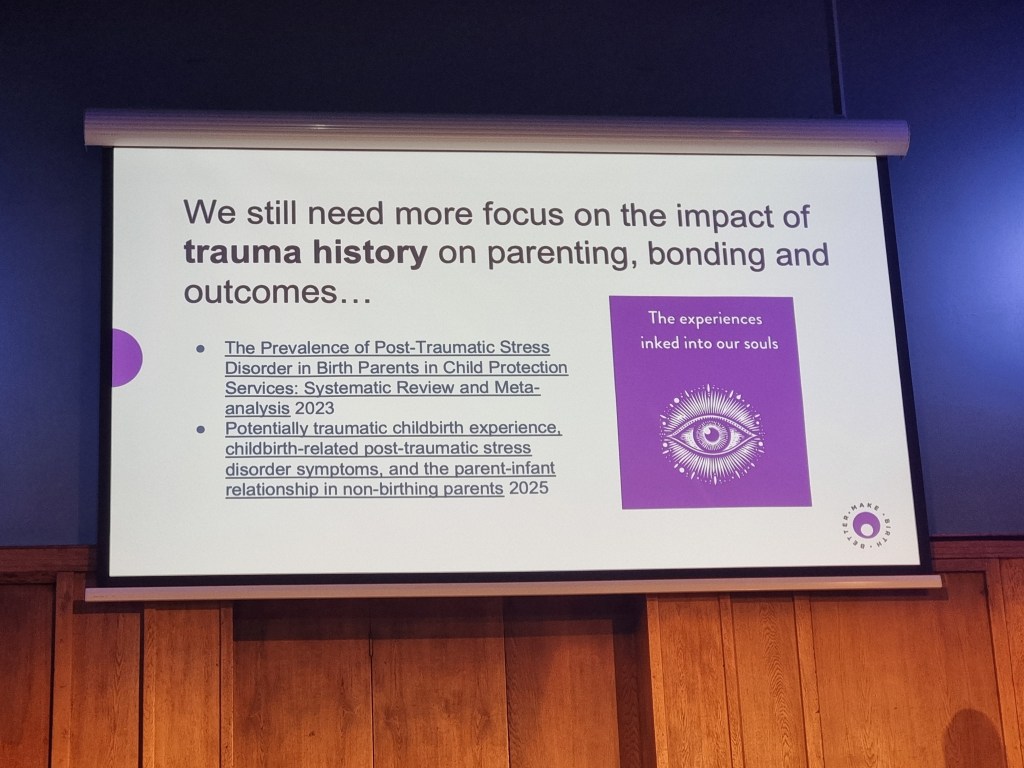
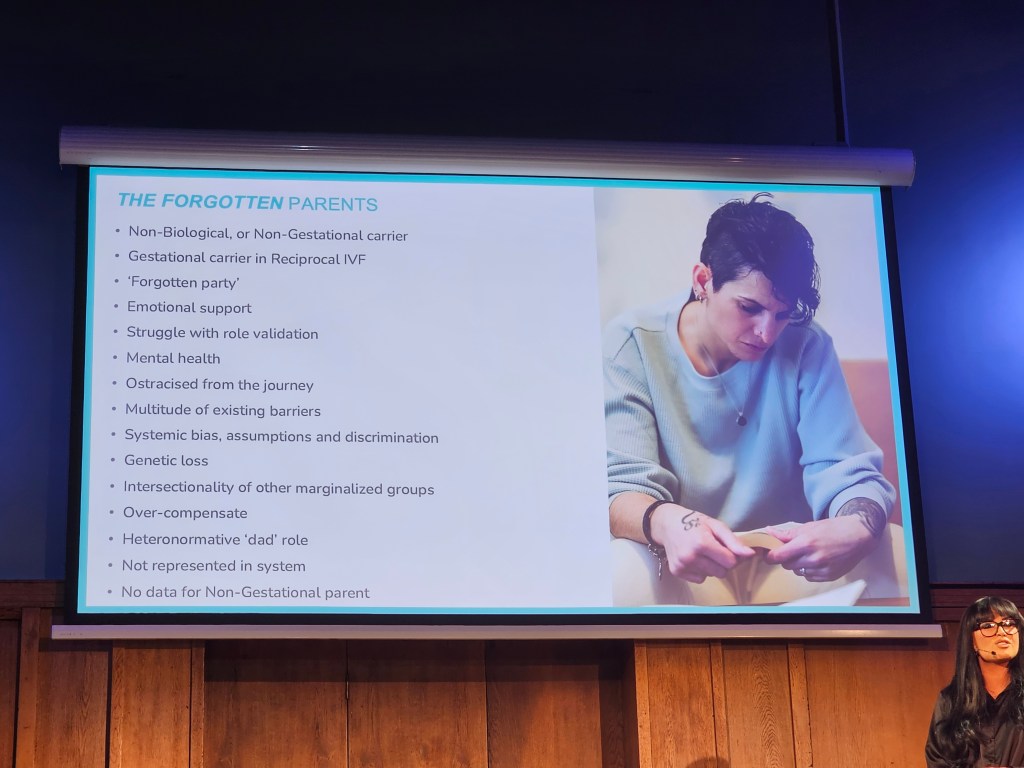
2) Validity to all voices – the discourse surrounding the experience of so many people continues to either be reductive, distorted, or overlooked. These people include non-birthing partners, babies, and people from minoritised racial, ethnic, religious, class, gender and sexual backgrounds. It is an injustice for their experiences to remain missing, ostracised and erased, and it was great to hear much discussion around this. I asked panel members a question about having men present at such summits (there was probably 2/3 men out of 200 people present) which had a fairly positive response. ALL people want to be involved (at minimum acknowledged) in these conversations because they have experience, it impacts them, it MATTERS to them. Yet as much as recognition talk is great, it needs to be backed with concrete actions.
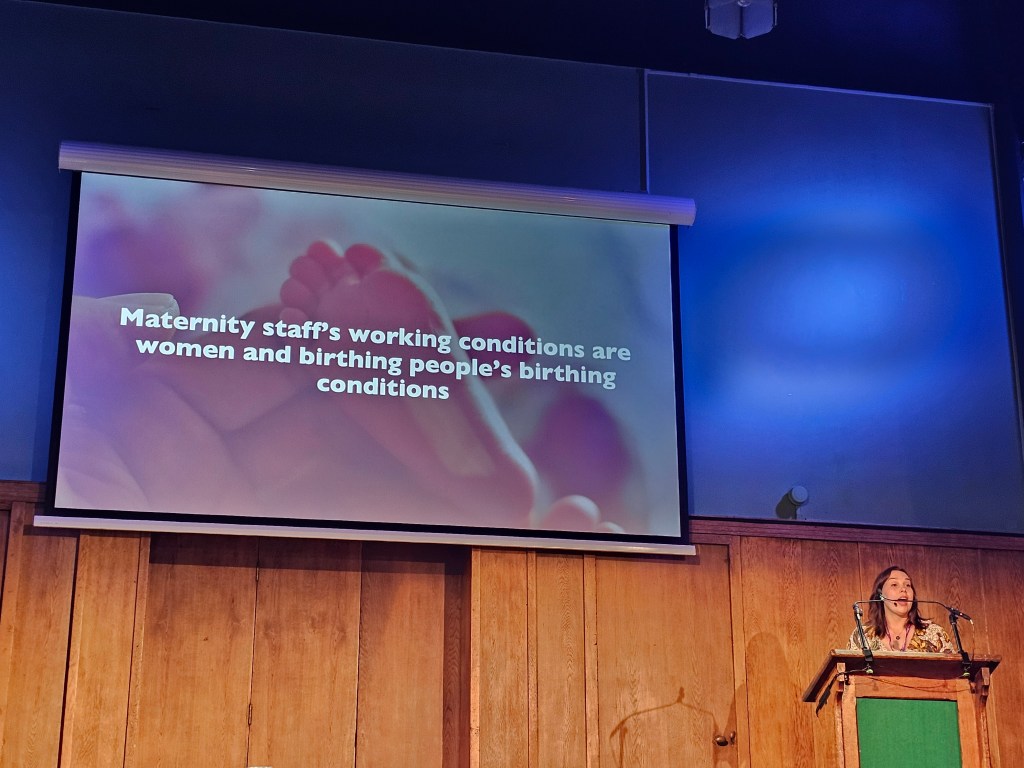
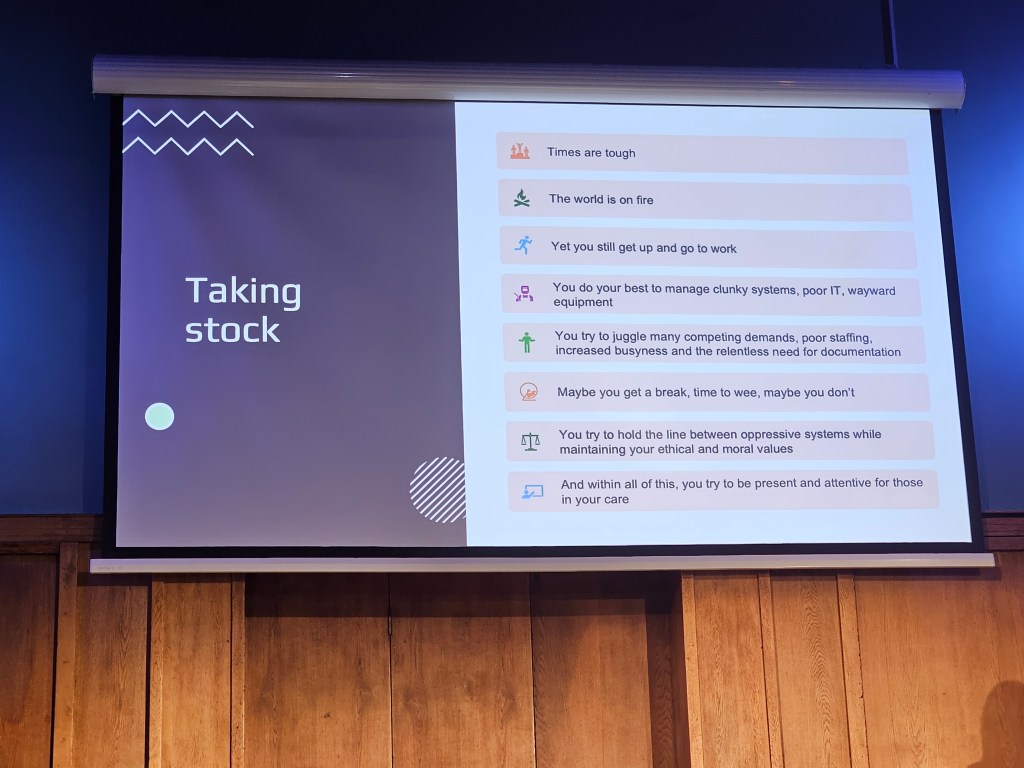
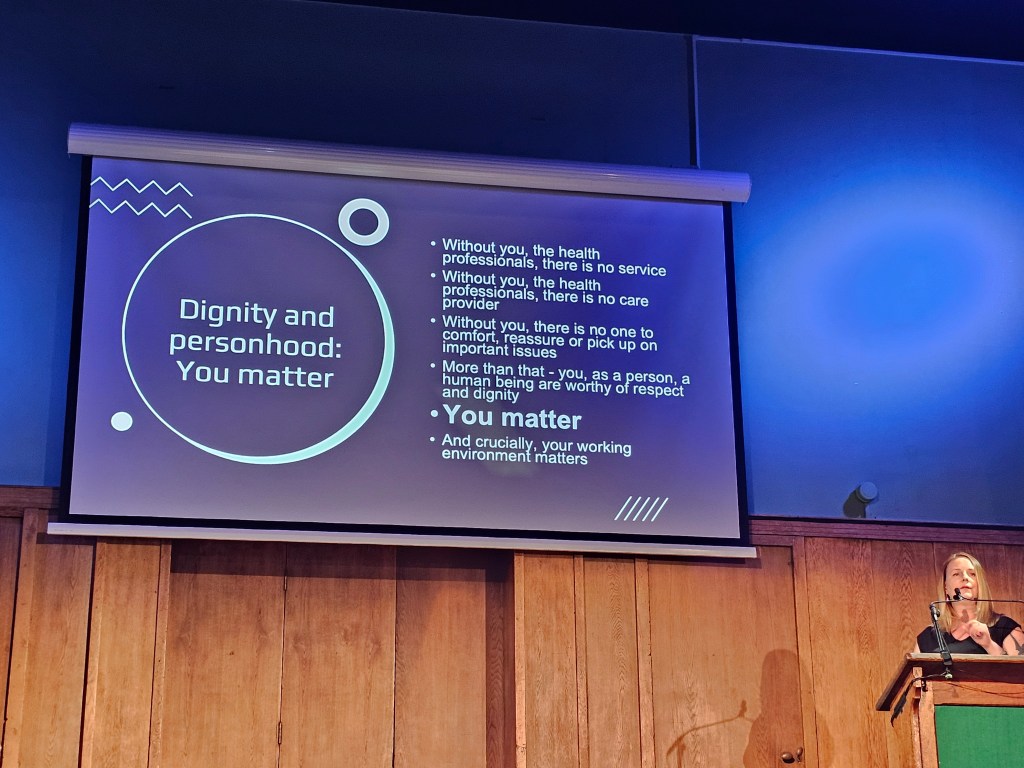
3) Staff empowerment – healthcare workers want to provide the best care possible, and systems don’t only oppress patients, but also the staff that work in these systems. We continue to be let down by cultures + systems disregarding emotions, trauma and human agency, including through insufficient training and limited compassionate support. The impact of different social, cultural and political dynamics need to be recognised and understood better, and more compassion and empowerment is needed for staff. I have long believed this, and it was reaffirming to meet many people who share these views.
4) Collaboration – there’s huge scope for collaboration between healthcare providers and workers across different fields. As a Paramedic I agree that ambulance services need to be recognised as a system partner in maternity care, but I’m also speaking about collaboration around emotional wellbeing and performance. We have countless commonalities in the performance of our roles and wider practice. For instance, I didn’t need additional explanation and context from many speakers because I could resonate with the experiences they shared of clinical and non-clinical dynamics of healthcare. There are common principles in good and bad practice throughout healthcare, and we can learn from and grow with each other.
5) Ambulance Services – I have seen how the most vulnerable people are likely to access ambulance services. I also agree that frontline staff are passionate and enthusiastic about providing optimal care yet often find this area of healthcare challenging. But the view that new guidelines, algorithms and screening tools are empowering is far-fetched. These may capture the physiology and experiences of birthing people better, but they don’t enable staff to exercise more control and have better understanding of the clinical and non-clinical dynamics of maternity-related encounters. More regular, hands-on clinical and non-clinical education and training is needed to truly and effectively empower staff, including greater awareness of the wider human experience of people’s fertility and maternity journeys.

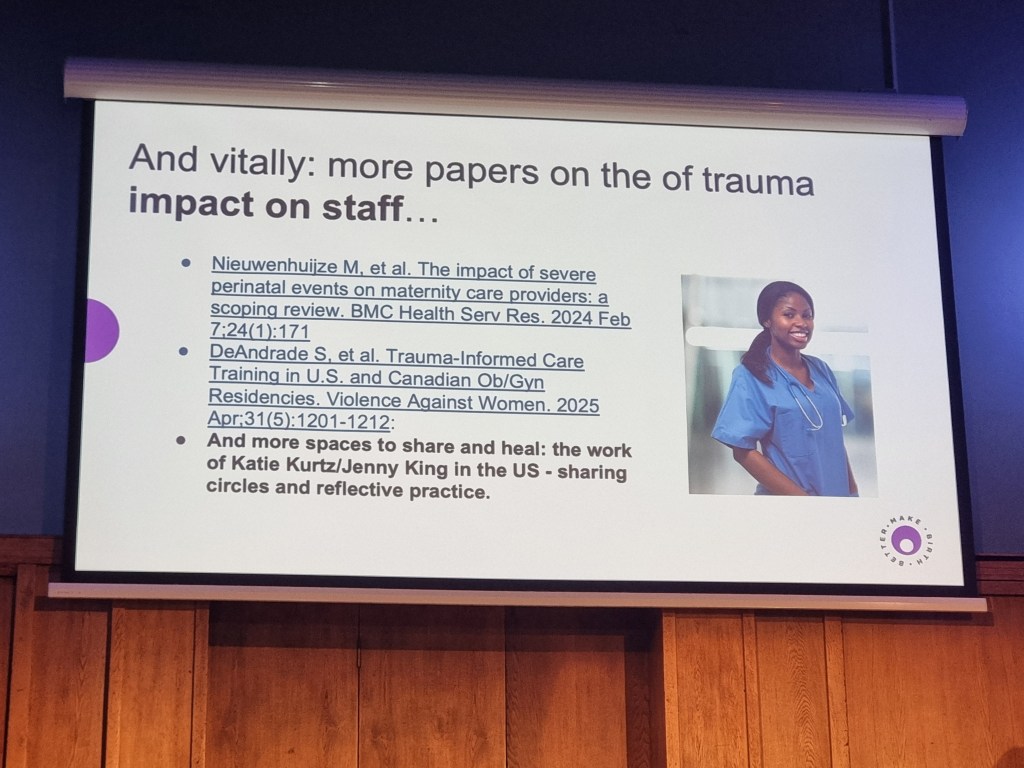
6) Future developments – despite legal changes surrounding informed consent and patient engagement/empowerment, the agency of birthing people continues to be neglected and dismissed – this can’t continue. It is vital in enabling the prevention of perinatal trauma, as is substantive, trauma-informed ante-natal education, compassionate support for staff and continuity of care across services. Although gaps remain in perinatal trauma research, more specifically relating to minoritised groups, the long-term human experience and constructive effective actions/strategies in managing trauma – we already know plenty. There is an abundance of existing knowledge and experience that we can draw upon to effect change and prevent/manage perinatal trauma more effectively.

7) BY DEFAULT, NOT AFTER FAULT – this was probably my favourite quote from a speaker/panelist throughout the whole summit who spoke about providing inclusive and empowering initiatives! A societal issue I have long seen since I was young is an obsession of cure vs prevention. We keep REACTIVELY creating new initiatives, policies, projects, tools and campaigns to deal with consequences of ineffective systems and cultures rather than address the root causes of many issues. In the context of perinatal trauma, as much as there is a need for further training, education, resources and support, requisite changes, values and actions need to be INHERENT in practice. They need to be incorporated into how we perform healthcare, rather than an after thought. We need to proactively empower people and practitioners, incorporate and integrate these principles into our training, cultures and systems to prevent harm and trauma. Simply picking up the pieces of poor practice in not only unsustainable, but UNJUST. All human lives deserve more dignity and respect.
What’s next?
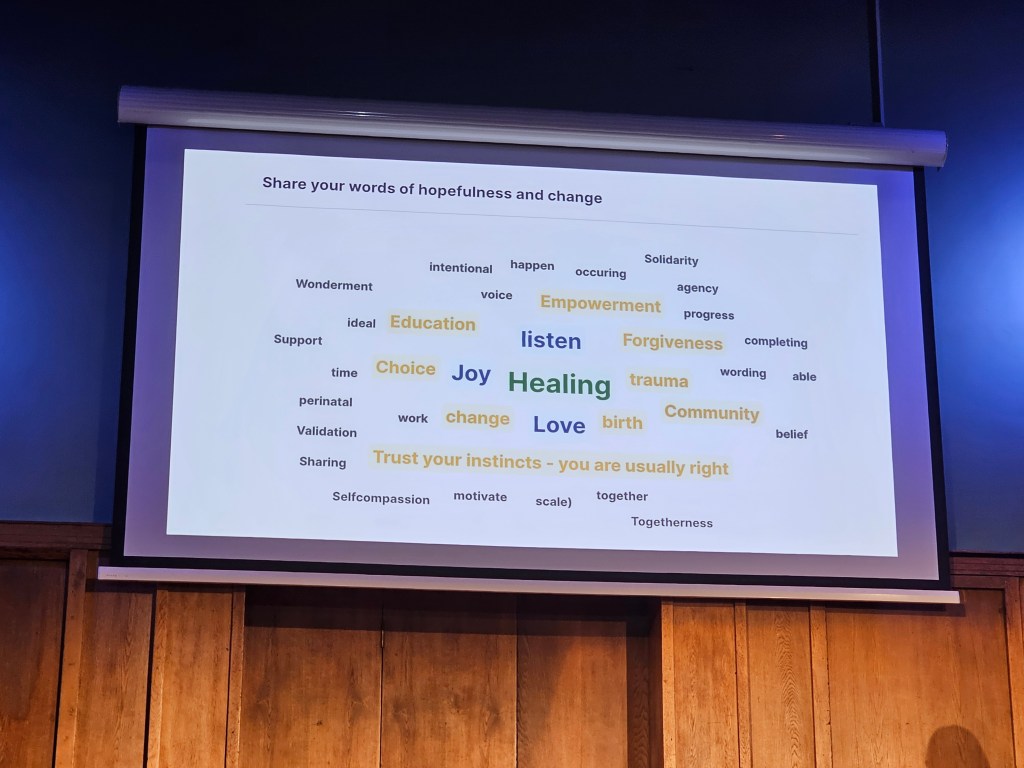
This summit underlined and endorsed my strongly and deeply held view that emotional wellbeing is paramount to humans. This includes, but isn’t limited to, people freely exercising their agency, experiencing belonging, and having their identities valued and respected. Moreover, humans have varying capacities to express, regulate and process emotions. Developing these capacities, empowering people to exercise these effectively, can enable us to live and lead better lives. This is something I would love to do for people, and my journey is about developing ways to achieve this.
In relation to healthcare, I feel motivated to continue my work in emotional wellbeing and performance as I know I’m not the only who has such ideas and insights, and there are allies in healthcare advocating for similar changes. I want to engage with the space of perinatal trauma more because I feel I have much to contribute and learn – it would be an incredible exchange.

We keep doing what we can, where and when we can – we keep going.